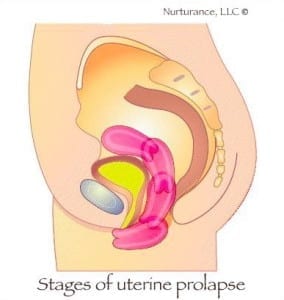
Uterine prolapse is when the womb (uterus) descends from its normal position into the vaginal area. There are four stages of uterine prolapse. First-degree uterine prolapse is when the cervix drops into the vagina. Second-degree prolapse is when the cervix sticks out of the opening of the vagina. Third-degree is when the cervix is outside of the vagina and fourth degree is when the entire uterus is outside the vagina.
Cystocele is when part of the bladder bulges into the vagina. Rectocele is when the rectum bulges into the lower rear vaginal wall. This can make bowel movements difficult and women may need to push on the inside rear wall of the vagina with their fingers to empty the bowel. Enterocele is when a portion of the small intestine bulges into the vagina through a herniation in the rear upper portion of the upper rear vaginal wall.
Prolapse can be a result of a weakness or tension in the supporting structures of the organs such as muscles, ligaments, and fascia. The weakness can be caused by lack of proper alignment of the pelvis, sacrum, traumatic falls or accidents, emotional component/trauma, spleen qi deficiency, kidney yang deficiency, and from using the excessive Valsalva maneuver. Valsalva is when you take in a breath, seal it off and push to get things like poop, babies and snot out. Excessive pushing (Valsalva) causes unnecessary intra-abdominal pressure and can lead to damage of the supporting tissues. Also, overly tight pelvic floor muscles or scar tissue can create a downward pull on the pelvic organs. Other risk factors for prolapsed organs may be low estrogen levels, excessive pushing during birthing, forceps delivery, prolonged labor, chronic steroid use, and connective tissue disorders like Ehlers-Danlos or Marfan syndromes.
“The human body has great equipment for expelling various items. Smooth muscle creates wave-like motions that move items through the body (like food through your digestive tract, or particles up through your sinuses). Specialty muscles like the diaphragm (generating upward forces for coughing and vomiting) and the uterus (vaginal delivery) are well-designed and can really get the job done for you,” Katy Bowman-bio-mechanical scientist. Read more here about the over-developed habits that we have created that work against our natural expelling mechanics, making elimination of all types more difficult.
Click here and scroll down to page 80 to see imaging of prolapse of the bladder and uterus post-defecation Valsalva. (1)
Symptoms of prolapse:
- Heaviness in the pelvis
- Pelvic pain
- Constipation
- Urinary Incontinence
- Urinary frequency and urgency
- Lower back pain
- Difficulty walking
- Protrusion of tissue
- Difficulty urinating
- Difficult or painful intercourse
- May feel like you are sitting on a ball
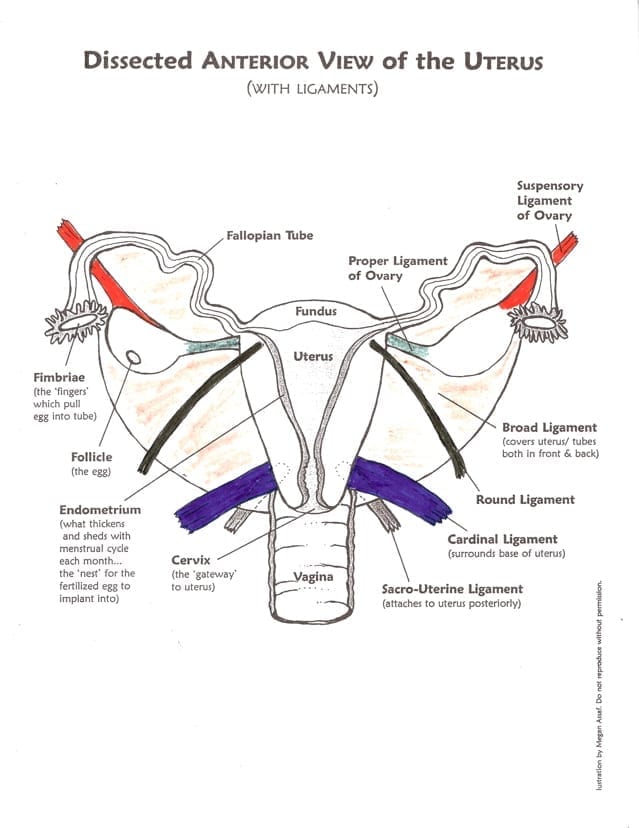
permission granted by illustrator Megan Assaf. Coloring by me : )
Help for prolapsed uterus:
The following information is for educational and resource purposes only.
1. Stop sucking in. See my video demonstration on where your organs go when you suck your belly in. Seriously, This is important! I also consider the act of constantly “engaging the core” by pulling your belly to the spine, sucking in and pushing the organs out. You shouldn’t have to consciously “activate the TVA” for everyday tasks when you are in alignment.
2. Restorative Exercise for whole body alignment. I teach these restorative exercises for pelvic floor health in my Womb Care course. I always, always, always include restorative exercise with my clients suffering from a prolapse. Whole body alignment is crucial. No one area of your body works in isolation!
3. Address constipation so that you stop straining during bowel movements. To do this you may have to follow steps one and two, drink enough water and talk to a qualified practitioner about your diet. Sometimes drinking one or two glasses of water with lemon, first thing in the morning will help flush the colon (lemon stimulates bile which is a natural laxative). If constipation is a problem for you please address the root cause. Read Constipation: A.K.A. Log Jam for helpful tips.
4. Learn self-care massage to lift the uterus. The technique is a noninvasive external technique designed to lift and center the uterus and improve blood and lymph flow. If you do not have a practitioner near you, I teach a form of uterine massage in my Womb Care Online course. I can also teach you via Zoom. Do the self-care massage on a slant board (about 45 degrees) or pillow that puts your hips higher than your head, this will allow gravity aid you during self-care.
l have seen excellent results with women who have stage one and two prolapses, and moderate to good results in stage three prolapse (once a complete reversal) with diligent self-care massage and alignment awareness.
5. A Visceral Manipulation™ practitioner who has completed VM3 should also be able to help. I have done both trainings in the Arvigo® work and in Visceral Manipulation™-they are both vastly different in their approach. The techniques I use depends on the individual situation.
6. No lifting over 10 pounds while you are healing if you are not able to lift without the Valsalva maneuver (creating internal pressure).
7. Homeopathics “A disturbance in the balance of Calc. fluor. or Calcium Fluoride in any of the body tissues can cause a chronically relaxed condition of any of the associated tissues,” from the Natural Health DOC website. Sepia is a homeopathic remedy geared toward the physical and emotional feelings associated with uterine prolapse. Typical Dose: 3 pellets of 30x.
*There is a homeopathic suppository remedy for prolapse, homeopathy can be very specific to the individual, so it’s best to see someone who specializes in homeopathic medicine.
8. Nourish Zinc and Vitamin C help tissue healing and integrity.
One of my clients reported improvement with her prolapse after receiving IV vitamin C therapy, so I asked Dr. Kaley Bourgeois at Lake Oswego Health Center whether vitamin IV therapy can help women with uterine prolapse. She stated that “Vitamin C therapy can be helpful with supporting tissue integrity, but I’ve found ozone intravenous therapies to be more effective. Most likely due to the increased oxygenation of tissues via the blood. Often we combine by starting with the ozone therapy, followed by a smaller vitamin push.” She also said that Bio-identical hormone support is sometimes helpful as well when appropriate.
9. Holistic Pelvic Care™ “covers the female energy system and working with organ energies, the physical body & mapping internal pelvic tension patterns, and creative energies & trauma: restoring equilibrium in the pelvic space by working at the energy/body interface.” (source)
In the case of pelvic organ prolapse many people assume the pelvic floor is weak, hence the obsession with Kegel exercises. However, overly tight pelvic floor muscles or scar tissue can create a downward pull on the pelvic organs. Intra vaginal pelvic floor physical therapy can help reduce tension and rebalance how the pelvic floor functions. Remember tension does not equal strength.
10 Ask for help when needed. Many women with prolapse organs report that they lack adequate support from their loved ones or coworkers. This is especially true with new mothers. We aren’t meant to do it all alone. Remember some people may not know you need help unless you ask.
11. Acupuncture or acupressure to certain points to raise the organ qi or treat deficiency. GV20 is perhaps the point most well-known for the treatment of prolapse. Located five cun within the anterior hairline on the governing vessel channel, it has the ability to raise the yang. A cun is the distance between the distal and proximal interphalangeal joints of the middle finger and is used as a measuring tool to find acupuncture points. Prolapse can have several sources, so see a qualified acupuncturist for a proper diagnosis. Chinese herbal medicine also has several herbal formulas for uterine prolapse.
12. Moxa on these points.
13. Transition to zero drop shoes (the heel of the shoe should be at the same altitude as the ball of the foot). I can’t stress how important this is for pelvic floor health. How you transition to a zero drop shoe is also important, so don’t just throw out all your shoes just yet. I recommend this book to safely transition to minimal footwear.
14. Manage your general health, including alternative modalities and using conventional health care when needed. In some cases, especially stage four prolapse, a pessary may be used. A pessary is a small plastic or silicone medical device which is inserted into the vagina and acts as a support. You can see the different types of pessaries and how they are inserted here.
Resource:
1.Imaging Pelvic Floor Disorders
By Jaap Stoker, Albert L. Baert, Stuart A. Taylor, John O.L. Delancey






Would you consider maybe doing some sort of online course in the self-care massage? I know that probably isn’t optimal, but I don’t think there are any arvigo massage practitioners in my entire country. And I’m a bit desperate to learn this…
Hi Hanna, I do teach an online course called Hands on Health, Healing the Maya Way. The next scheduled class is in June. See the link here, https://alignmentmonkey.nurturance.net/hands-on-health-healing-the-maya-way
The class is six hours split up over three Saturdays. If you are not interested in learning all that is offered in the class and just want to learn the self care massage I can teach you via SKYPE.
Fantastic information! I think a lot of women look to kegels or surgery to correct prolapse and it either doesn’t work or it’s unnecessary (at least for more minor cases).
Have you looked into the Tupler technique to help correct diastasis? When the abs are seperated (thanks to pregnancy and / or sit-ups and crunches) the entire area is weakned and prolapse as well as incontinence becomes a problem.
This is a great blog, glad I came across it.
Thank you Darlene. Diastasis recti isn’t actually caused from pregnancy, men get it as well. Diastasis recti is an issue of poor physical alignment that one had before getting pregnant. To correct the issue, would be a matter of correcting your alignment . When one can maintain a neutral pelvis and keep their ribs dropped in vertical alignment over the ASIS, the body can naturally repair itself on it’s own and maintain normal intra-abdominal pressure to avoid the D.R. in the first place.
I am interested in learning the self care massage that you teach, but not really ready for an entire course. Would you be able to skype a session with me? (I am a RES jsyk)
Absolutely, I can teach you via Skype. I take Skype appointments on Tuesdays.
Excellent
Keep up the good work
I’m not familiar with ‘skype but I do FaceTime. Is that a possibility for learning the self care massage?
Do you still teach massage techniques? I’m interested in learning how to do this to help raise my uterus back up. I’m you and just had a baby causing my uterus to prolapse to a moderate degree.
Hi Susie,
I could do FaceTime instead of SKYPE. I don’t teach the Arvigo self-care online (only in person), but I could teach you the Chinese Abdominal massage self-care and Restorative Exercise™ for prolapse and pelvic floor health via Skype/Facetime.
Hi Sierra, Yes, I still teach the massage techniques. I teach one-to-one in person in Portland, Oregon http://nurturance.net/, or via the self-care Arvigo level one classes. https://alignmentmonkey.nurturance.net/classes/
I can also teach the Chinese Abdominal massage self-care and Restorative Exercise™ for prolapse and pelvic floor health via Skype. https://alignmentmonkey.nurturance.net/skype-2/
Hi Barabara,
I am feim Aruba
I would like to skype with you
Need advices on prolapse
Tamara
Hi Barbara,
Is it possible to non surgically correct/recover a stage 3 prolapse from your experience? Have any clients of yours reported that the heaviness feeling of prolapse goes away after surgery?
Thank you.
I’ve had excellent results with stage 1 and 2 prolapse and moderate results with stage three. However, I’ve seen complete reversal of stage 3 uterine prolapse using abdominal therapies, nutrition, and Restorative Exercise™.
In regards to your second question, it depends on the type of surgery. With a hysterectomy,the bowels will descend to where the uterus was and may cause heaviness. If you’re thinking about getting a hysterectomy you may want to check out the HERS Foundation website for a complete list of possible effects. http://www.hersfoundation.com/effects.html
I have been diagnosed with a Rectocele and Cystocel after giving birth.Specialist and Physio say its a grade 2 rectocele and a 1.5 Cystocel. I have been considering surgery but really would like to avoid it. I would like to take the natural route if possible. Can Visceral Manipulation fix a prolapsed bladder and bowel? I would like to completely reverse it if possible. With a little one I do not want to be down after surgery for 8 wk recovery and I understand alot of women have to go back for another surgery 5 or so years later. If you can recommend any other techniques or modalities it would be greatly appreciated. TIA.
Hi M. Yes, I believe it can be reversed. In my practice, I would probably do a combination of Visceral Manipulation™, Arvgo® therapy, and restorative exercise/whole body alignment work and maybe some of the other things I mentioned in the article.
What’s going on in the feet and legs can affect the pelvic organs. https://alignmentmonkey.nurturance.net/2016/your-bladder-is-connected-to-your-leg-bone/
Of course, nutrition, proper rest and other factors come into play. I don’t know how old your little one is, but it may take 2 years for ligaments to completely heal.
Hello Barbara
I have a 2nd degree uterine prolapse and I live in a country where there is almost no womens health PT. Can you treat.me online? If not what do you recommend. I’m desperate for help; feel I am all alone
Thank you
Hi Hala, I’m sorry to hear you aren’t getting the help you need. In general, I believe women can improve their uterine prolapse doing self-abdominal massage and pelvic alignment exercises. I don’t offer skype appointments, but I do have an online Womb Care course that covers self-massage and pelvic alignment. You can read about it here: https://courses.nurturance.net/sales-womb-course/
Thanks a lot Barbara for your prompt reply I really appreciate it. I have another question if you do not mind. Do you think it is possible for me to reverse my second degree uterine prolapse given that it has been two years and a half since I developed it? I have been looking for help ever since I developed this condition with little success. Here in Egypt, where I live, only surgery is available for treating prolapse.
All the Best
Hala
I forgot to thank you for letting me know about your online course. I will buy it as soon as I can. I am sure it is full of a wealth of great info. When is the next discount?, I missed the Mothers day discount. Is it available as a download?
Thank you